NPL research provides new insights into analysing kidney tissues for patient transplants.
The National Physical Laboratory (NPL) announces findings from two studies on the methods used to assess the health and suitability of kidneys for transplantation, which could potentially help to increase the number of available transplants. The studies have been published in the journals Transplantation Direct (Transplantation Direct (lww.com)) and in Frontiers in Nephrology ( Frontiers | Quantifying measurement uncertainty in renal transplant biopsy assessment (frontiersin.org)
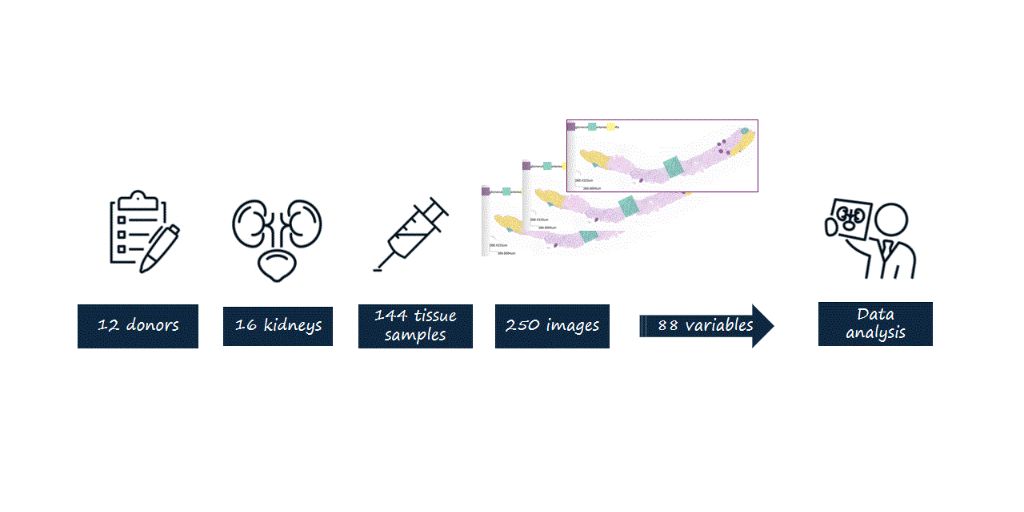
Scientists and clinicians from NPL and the University of Cambridge completed two studies on improving the kidney health assessment. The research involved taking repeated measurements on tissue samples taken from 16 discarded kidneys (kidneys considered, but not used for transplantation) using six different ways to prepare the tissue and comparing the results.
Current indicators of donor kidney health for transplantation focus on the donor’s age and clinical history. This approach can lead to organ waste due to discarding potentially healthy kidneys, most often from older donors.
For the first study, the scientists measured features such as scarring or blood vessel health on the kidney tissue samples and calculated multiple scores for each kidney to understand the magnitude and patterns of variation. The scores predicted whether the discarded kidney would have been healthy enough for transplantation. The researchers found that more than half of the discarded kidneys were fit for transplantation and that the scores differed significantly by chance and depending on how the kidney tissue was prepared.
This discovery led to the second study, where the NPL scientists aimed to find which measurement methods could predict the kidney’s suitability for transplantation more reliably. The scientists looked for the best way to prepare and analyse the kidney tissue and provided several recommendations to help clinicians calculate more reliable health scores. One recommendation is the optimal size for the surface area of kidney tissue that yields reliable measurements while minimising injury to the kidney.
NPL scientists will conduct deeper research into how tissue samples should be taken and analysed, as well as which kidney areas are more suitable for tissue sampling. This will enable them to make further recommendations to help clinicians maximise the impact of tissue assessment in the transplantation process.
The scientists working on these papers Dr Xavier Loizeau, Dr Spencer Thomas and Dr Marina Romanchikova said: “Hopefully, the findings of this study will help design a trustworthy organ selection process for previously unconsidered donors, addressing the current shortage of kidneys for transplantation.
This work demonstrates how metrology can help solve the challenges of reproducibility in science. Here we provide insight into the quality and reproducibility of clinical measurements laying the foundations for defining good practice and standardised measurements, improving clinical decision making and ultimately patient outcomes.
This study shows how measurement science can support clinicians by using the principles of experiment design to study what affects the biopsy score.”
Dr Alex Samoshkin, Deputy Head, Office for Translational Research, University of Cambridge, added: “These findings have very important translational impacts, that consider an organ fitness based on its structural features, rather than on “nonspecific parameters” like age. In fact, in today’s world, several senior men and women are in very good health, therefore their organs could be perfectly suitable for patients.”
Mr Tobi Ayorinde NIHR Clinical Lecturer in Transplant Surgery, UCL said: “How we measure organ quality in transplantation is crucial, as it forms the basis for decisions made by doctors and patients. Our findings demonstrate that by improving on the fundamentals, we can increase confidence and potentially expand the pool of viable organs, giving more patients the opportunity of a successful transplant.”











