Hybrid operating rooms are predominantly used by cardiovascular disciplines, but as the demand for gentler surgery methods increases, we can expect more sub-disciplines to make use of the technology. A hybrid operating room is a costly expense and there are several considerations that must be made for the investment to be a true success, as Steve Hughes, managing director of medical power quality specialist REO UK, explains.
The World Health Organisation (WHO) predicts that by 2050, the worldwide population over 60 will have doubled to reach two billion people. Driven by falling fertility rates and an increase in life expectancy, the growth of the ageing population is expected to not only continue, but accelerate in the coming years. The concern, however, is that as we age, we become more susceptible to illness and infection.
Today, chronic conditions like diabetes, cancer and cardiovascular diseases account for an estimated 77 per cent of the disease burden and 86 per cent of the deaths across Europe. As such, an ageing population inevitably increases the volume of hospital admissions and practitioner appointments, placing significant pressure on healthcare systems.
Now, if you told an NHS director of finance that they could reduce patient operating times and reduce the time that in-patients spend in hospitals, they’d most likely snap your hand off. This could soon become a reality with the wide adoption of hybrid operating theatres, which is expected to grow at significant pace between now and 2023.
So, what are hybrid operating rooms? While they may sound like they come from a sci-fi novel, the operating rooms have been implemented in NHS hospitals across the UK, such as the St George’s University Hospitals Trust in London. Many NHS managers may soon be considering investing in them for their own hospitals.
Flexible imaging
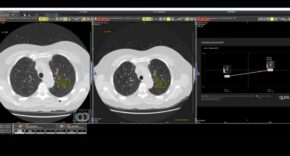
Hybrid operating rooms combine both the traditional operating theatre with high-end imaging systems such as magnetic resonance imaging (MRI), computed tomography (CT) scans or angiography systems.
Previously, only mobile imaging equipment was based inside an operating room in the form of C-Arms, ultrasound and endoscopy. However, the quality of the images created by this equipment was often not high enough to base surgical procedures on.
For example, mobile angiography systems have a lower image quality due to lesser tube performance and a low refresh rate. This is problematic for endovascular cases where surgeons need to see the smallest blood vessels.
In the past, the patient would have to be wheeled out of the sterile environment of the operating theatre and taken to the imaging department. However, in the hybrid operating theatre, an intraoperative 3D imaging system can be continually used to guide the surgeon.
This follows the trend of minimally invasive surgery (MIS) that we recently identified in our state of medical technology report. This is where surgeons try to reduce the trauma involved in surgery by minimising the size and frequency of incisions. For example, surgeons can carry out vascular surgery for aortic aneurysms without the need for open chest or abdominal surgery.
In emergency situations, patients with severe bleeding need immediate care to avoid life-threatening blood loss. Hybrid operating rooms allow doctors to perform open and endovascular treatment without having to reposition the patient, which could result in further injury. So, in the event of a patient experiencing tension on the brain due to a severe haemorrhage, doctors can relieve the tension and coil an aneurysm in the same room.
The reduced trauma helps to reduce the risk of complications, lowers patient recovery time and shortens the average length of hospital stays after the procedure. However, before hospital managers jump at the chance of this, they must consider the complications of bringing so many pieces of equipment together.
In fact, design and electrical engineers in the MedTech and healthcare industries are pivotal to ensuring the safety of patients as modern hospitals become more technologically advanced.
Electrical considerations
Most hospitals in the UK typically follow procedures to reduce the interference caused by medical equipment and comply with regulations such as the European standard EN60601, which outlines the basic requirements for medical equipment in hospitals. Even with these standards in place, extra precautions should be taken, especially with the integration of hybrid operating rooms.
“These are complex projects with high-end equipment and interdisciplinary collaborations,” explains Jane Whittaker, angiography business manager at Siemens Healthcare. “There can be an increased number of people working within this environment, as well as a wide range of equipment required for the procedure. From our experience, the most successful installations are the result of careful planning and strong communication between all stakeholders throughout the project.”
An important point that all parties should consider is power quality and the problems that can occur with so many different electrical requirements in a single room. With imaging systems and traditional monitors in an operating room, design engineers must consider the additional power quality implications of this compared to a traditional operating room.
To protect patients, hospital managers must consider all the equipment used in their hospitals as a whole. MRI scanners, for example, emit large amounts of electromagnetic radiation and without taking the necessary steps to ensure radiofrequency shielding, the electromagnetic radiation could cause interference in nearby medical devices.
If the levels of electromagnetic energy exceed the electromagnetic resistance a device has been designed and tested for, then this can result in electromagnetic interference (EMI). Hybrid operating rooms are susceptible to issues like EMI because of the high usage and range of power electronics-based medical equipment in one room.
If unaddressed, EMI causes electrical harmonics, spikes and fluctuations in power, which can interfere with the mains network causing intermittent faults, short circuits or even a complete power outage. This can impact the data collected by medical equipment and the way devices interact with each other. If decisions are being made on the basis of potentially incorrect data given by the equipment, this could prove dangerous for the patient.
For critical systems that are taking measurements or displaying essential images, any electrical interference in the mains supply could affect the performance of the equipment. This can accelerate the wear of components, increasing the chances of device failure and putting patients at risk.
When designing electrical equipment to go in hybrid operating rooms, engineers must therefore incorporate components to reduce the effect of electrical interference.
An important way to do this is by using isolating transformers such as REO’s REOMED range. The wide REOMED portfolio includes radio frequency interference (RFI) filters, surge protection and protection against half-wave loss. These products are specially engineered to go above and beyond the required medical standards such as the European EN 60 601-1 standard for electrical medical technology.
When the transformers are used in operating theatres, they allow safe galvanic separation between the primary and secondary circuits. This limits interference from other devices in the operating theatre, as well as protecting equipment from poor power quality.
Traditionally, some engineers are put off by electrical transformers for medical environments, as they tend to have quite high electrical losses. This reduces energy efficiency, which could negate the cost savings made by reducing patient costs with hybrid operating theatres. However, REO UK’s REOMED transformers have been shown to deliver a 45 per cent reduction in electrical losses compared to conventional electrical transformers.
While hybrid operating rooms present a wealth of new possibilities for healthcare, they bring with them the challenges of equipment safety, power quality and system continuity. These can only be safely overcome with the expertise of design and electrical engineers, as well as power quality specialists.
Therefore, to reap the benefits that hybrid operating theatres bring to hospitals and patient, it is vital that design engineers consider the implications for power quality in this new type of environment. If they fail to consider the need for isolating, engineers may negate the cost savings made by the hybrid theatres and decrease the quality of patient care, rather than increase it.
While the adoption of hybrid operating rooms has been slow, as the concept was first introduced in the 1990s, the increase in complex surgical procedures means we can expect the integration in hospitals of at least one hybrid operating room to continue to increase.
This is only one instance of how design engineers can contribute towards improving power quality in healthcare settings. To find out how else design engineers can ensure their medical equipment is reliable, download our medical technology whitepaper from the REO UK website.