0
17th June 2024 10:00 am
NEW YORK — For people with a range of musculoskeletal (MSK) conditions, many virtual solutions deliver clinically meaningful improvements in pain and function, according to a new independent evaluation from the Peterson Health Technology Institute (PHTI).
Based on a rigorous, independent review of scientific literature, the evidence indicates that many of these solutions offer clinical benefits to patients that are comparable to in-person physical therapy (PT). These solutions also have the potential to improve access to therapy, reduce healthcare spending, and offer greater convenience compared to in-person PT.
Nearly one in three people in the United States have an MSK disorder, which are the leading causes of disability and account for nearly 10% of medical spending in the U.S. These conditions impair patients’ daily lives, impact their productivity, limit their ability to work and earn a living, and contribute to mental health challenges. Since 2010, more than $38 billion has been invested in companies offering MSK solutions, including mergers and acquisitions.
“We know that early and regular use of physical therapy can speed the healing process and avoid other complex MSK care, such as surgery. Our findings indicate that virtual solutions represent effective treatment options that can expand the number of patients who both start and stick with physical therapy,” said Caroline Pearson, executive director of PHTI. “These solutions leverage technology to efficiently and conveniently deliver services that help patients recover and avoid high-cost care, thereby reducing overall spending. In order to realize their full potential, virtual MSK solutions should be more closely integrated with medical care and insurance benefits.”
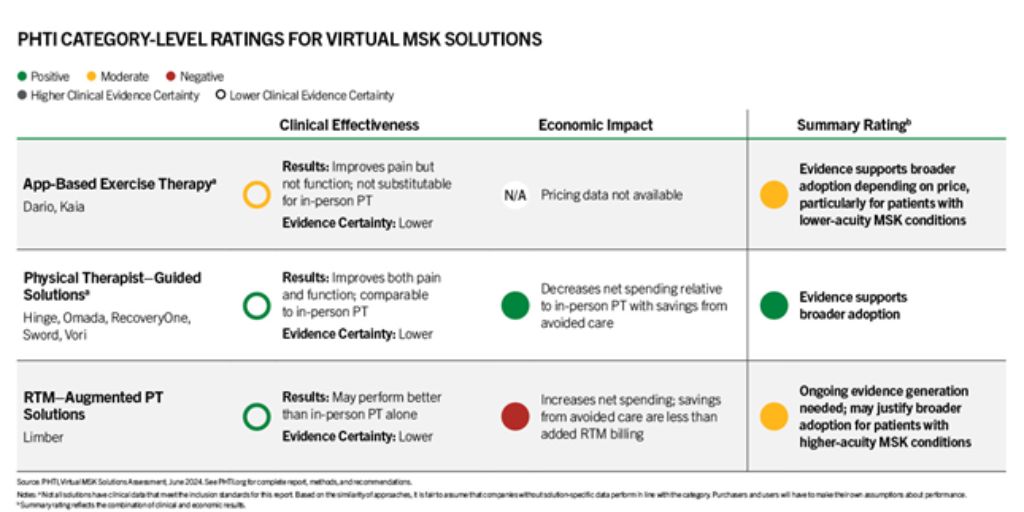
PHTI’s report assessed clinical and economic evidence on eight virtual MSK solutions in three categories: (1) app-based exercise therapy with limited physical therapist intervention, (2) physical therapist-guided solutions that are an alternative to in-person care, and (3) solutions that supplement in-person physical therapy with virtual care and are paid for as remote therapeutic monitoring (RTM). These technologies typically use body-worn motion trackers or cameras to guide patients through exercises and provide tailored feedback. The solutions in PHTI’s evaluation are sold by public and private companies, including DarioHealth, Hinge Health, Kaia Health, Limber Health, Omada Health, RecoveryOne, Sword Health, and Vori Health. The report focuses on virtual care for common MSK disorders, such as those that arise from acute injuries, repetitive motion or strain, or osteoarthritis.
PHTI’s analysis uses an evidence-based framework and review of more than 2,000 articles, including 53 submitted to PHTI by companies evaluated in the report. PHTI received input from various experts and individuals, including licensed physical therapists, clinical advisors, MSK patients, and other stakeholders. PHTI’s findings on clinical effectiveness and economic impact—as well as combined summary ratings for each category of solutions—are summarized below:
According to the findings, physical therapist-guided solutions offer the most promise and overall value, as they improve patient outcomes on pain and function comparably to in-person physical therapy, with a net decrease in spending. For many conditions, they may be reasonably substituted for in-person therapy. This category includes Hinge Health, Omada Health, RecoveryOne, Sword Health, and Vori Health. In terms of the economic impact, the report estimates that if 25% of in-person physical therapy users with low back pain shifted to these platforms at a price of $995 per year, annual savings could total approximately $4.4 million per one million commercially insured individuals.
“Treating musculoskeletal disorders can often be challenging. Many minor injuries will get better without any treatment, but early participation in rehabilitation exercises will get people back to exercise sooner with less risk of reinjury. Balancing these two facts while being mindful of costs is essential,” said report contributor Dr. Adam Bennett, Clinical Assistant Professor of Family and Community Medicine and Orthopedic Surgery, Northwestern University Feinberg School of Medicine.
“APTA applauds PHTI’s evaluation of physical therapy solutions to treat costly musculoskeletal conditions, including for populations who have limited access to in-person physical therapy,” said American Physical Therapy Association President Roger Herr, PT, MPA. “Virtual musculoskeletal solutions guided by PTs can help reduce overall health care costs, ease administrative burdens on physical therapists, close an access gap for millions, and deliver improved clinical outcomes for the patients under our care. APTA views this report as a call to action for payers and policymakers to enhance policies that harness the power of physical therapy through digital platforms, traditional in-person methods, and hybrid approaches.”
Additional topline findings from the report:
- App-based exercise therapies, including solutions from DarioHealth and Kaia, can improve pain and function compared to usual care, but are unlikely to be effective as total substitutes for in-person physical therapy. However, they may be effective solutions to provide broad-based virtual care for patients with lower-acuity who may experience clinical benefits, and the economic impact will depend on price.
- While there is a limited evidence base for RTM-augmented PT solutions used between in-person therapy sessions, the findings indicate that this category may deliver better clinical results on pain and functional improvement compared to in-person physical therapy alone. However, even after accounting for the health benefits these solutions provide, annual healthcare spending was estimated to increase because the savings from lower utilization do not offset increases in billing.
While virtual MSK solution companies seek to improve access to PT, their current business models are structured as employee wellness benefits that are disconnected from medical benefits and spending. This makes it more difficult for companies to quickly identify the patients who would benefit the most from care and approach them with their solution early in the treatment process. Virtual MSK solutions could deliver even better value by integrating into medical benefits, encouraging earlier referrals to PT, and actively managing other avoidable healthcare utilization.












