As the latest Health and Care Bill makes its way through parliament, Chris Barker, CEO, Spirit Health, reflects on key changes these reforms will bring about. Changes that will define the way industry engages with the NHS in the future; and a digital-first approach is at their core.
The recently published new Health and Care Bill formalises many of the structural reforms that have been taking shape over the past 18 months. It also sets in motion a wholesale change in the way the NHS makes decisions and allocates funding, outlined in three significant areas.
1. Whole system thinking
A new focus on system-based decision-making means that provider organisations now must take an active stake and interest in saving money on behalf of the whole integrated care system (ICS), which means weighing up a wider range of considerations than before.
Digital has much to contribute to this agenda. This could encompass providing easy access to the profile of patients that need treating or identifying where there may be pools of undiagnosed patients, defining health inequalities where cohorts of patients may not be receiving optimal care – or indeed, highlighting information gaps either for staff or patients.
In reality, however, what’s happening is that we are merging existing, non-digital structures. Therefore, where digital has a key role to play within whole-system thinking is integration. There are a vast number of digital solutions, of individual pilots and projects – and what we need is them all talking to each other. Integration and interoperability become vital in getting systems to seamlessly communicate, so that from a patient and clinician perspective, you can get the right information, at the right time, when you need it.
The other major consideration is that you can’t have a ‘whole system’ with digital data in silos. As it stands today, there is a significant divergence within the NHS in skill levels and comfort with digital solutions. In order to progress, we – as in both governing bodies and those providing the digital solutions – will need to invest in training and awareness as to what ‘digital-first’ actually means.
2. A shift to neighbourhood and place-based planning
Another shift involves the dissolution of the boundaries between primary and secondary care in favour of more integrated planning processes at neighbourhood and place-based levels as well as at a system level through ICSs.
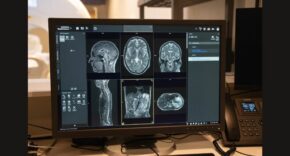
Digital solutions that place patients at the centre of their care; electronic care records that mitigate duplication of data between primary and secondary – as well as community – care, will be key to information decision-making at a regional and neighbourhood level. In addition, while the NHS will continue to battle with the long-tail of the COVID pandemic, digital solutions implemented at a regional and local level will play a significant factor in our ability to manage vulnerable patients, those with long-term conditions, and the potential peaks and troughs in cases and hospitalisations.
The challenge for our healthcare system here is that, in allowing for local adoption and implementation, we are likely to see 44 different place-based systems and 44 different debates as to what neighbourhood and place-based care actually means. Digital should be a means to collect, monitor and iterate on some of these solutions; a way to evaluate through digital methods what place-based care means for patients, for outcomes and how they can be improved.
3. Population health
The final shift involves the NHS moving beyond just thinking in terms of disease management and instead focusing much more on population health.
At system-level in particular, the NHS will increasingly be looking at how to support whole populations with certain health needs, particularly by improving diagnosis and intervening earlier to prevent demand on specialist services.
From being a core principle of the Long Term Plan, preventative health has now been given a structure and mechanism for delivery through the development of ICSs.
Aligned to this is the challenge of working with systems to monitor variation in pathways and supporting value propositions that can demonstrate clear economic value by unlocking cost-savings. Data that is unlocked through digital solutions will be a key success factor.
With so much data at our fingertips, the challenge lies in how we interpret that data, at the right time and in the right way for population health. And, looking ahead, how digital can enable us to – eventually – be predictive in terms of population health, at both a regional and national scale. This may not be something the NHS can achieve on its own; however, through collaboration between industry and provider organisations, we can ensure the right combination of technological / digital skills and clinical knowledge to bring about positive change.
Digital-first
No-one knows yet whether the changes in working practices of the last fifteen-to-eighteen months are likely to be sustained, but it is clear that as operational stresses increase, digital solutions have played a key role in protecting the vulnerable and NHS staff alike; from remote- and home-monitoring solutions for vulnerable patients with long-term conditions, to virtual learning platforms for others to help them better self-manage their conditions; and the establishment of virtual wards to manage early discharge post-COVID.
However, the phrase ‘digital-first’ is key. In order to ensure equality of access, we need to allow lots of options for other routes to care. Technology can be brilliant, but accessibility to healthcare must be universal.
Conclusion
There is an overarching need to embrace and support the new working realities within the NHS. The urgency can’t be overstated: the changes are here, they’re happening now and they demand our attention.
Yet, we can’t ignore the huge importance of managing this change successfully. We must help people with many different cultures and micro-cultures to embrace what is going to be a long journey. We must upskill both clinical and non-clinical workforces to help them become as close to digitally-native as they can be – because that is the only way to get digital-first thinking ingrained.