San Francisco, California; Helping to reduce claims inaccuracies and reduce admin waste, CoverSelf, a unified platform for healthcare claims and payment integrity, is today announcing a $8.2m seed round as it successfully deploys platform in the ecosystem.
The funding round was led by existing investors BEENEXT and 3one4 Capital with participation from new investor Z21 ventures and healthtech leaders. The fresh capital will be used to grow operations, build generative AI capabilities, and increase headcount in sales and marketing as the business scales.
The exponential growth of costs in healthcare remains a hotly debated and ever-evolving problem around the world. Over $4.1 trillion is spent on healthcare every year in the US alone, with administrative spending accounting for approximately one-quarter of the total amount. Founded in 2021 by seasoned US healthcare domain experts Rajasekhar Maddireddy and Raghavendra Pawar, CoverSelf aims to democratize the healthcare claims and payment integrity industry by creating a first-of-its-kind fully-open and transparent solution that empowers payment integrity teams in health insurance companies (payers) to transparently resolve health claims with hospitals and medical practices (providers).
“The current claims integrity systems are very complex, and the deployed technologies are antiquated. Significant software innovation is needed to address the broken system that is currently creating out-of-control healthcare costs and waste. The cobbled-together software solutions result in scattered data and the inability to make real-time business decisions. Administrative complexity costs billions annually, an open and collaborative platform can significantly reduce the repetitive administrative costs.” commented Rajasekhar Maddireddy, Founder of CoverSelf.
Over the last 12 months, the company has piloted the platform and successfully proved the platform’s readiness and effectiveness. This has translated to two deployments for insurers where the platform processes 25 times more claims in the same time window than was done earlier. Also, the platform has identified significant savings even after other vendors process claims. CoverSelf is in advanced discussions with 2 of the top 15 plans to collaborate. The current pipeline includes five of the top 15.
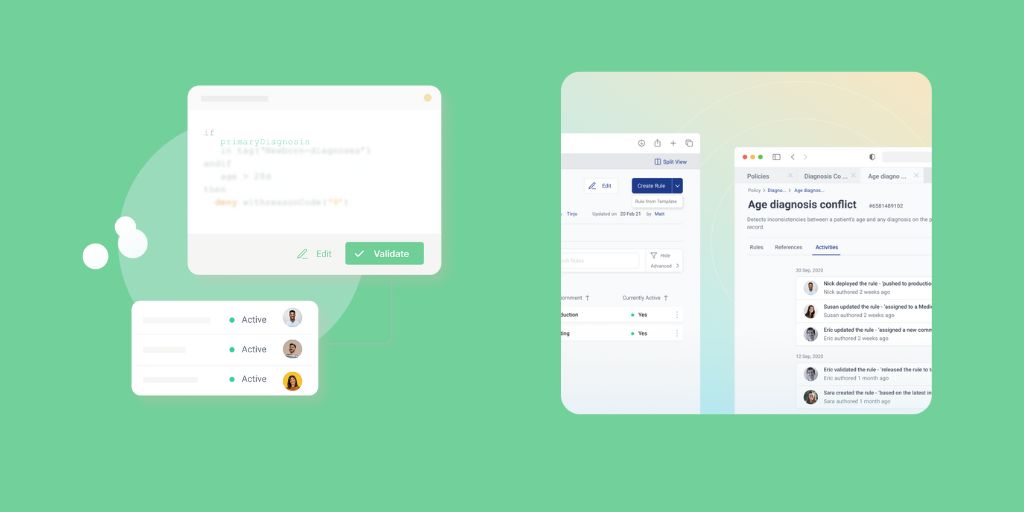
“One platform, one configuration, one team – our solution offers multiple points of integration and intervention for all pre and post-pay payment integrity, effectively reducing waste. CoverSelf is empowering subject matter experts (SMEs) with a modern UX/UI that’s super easy to work with and aids them by eliminating technical dependencies thereby maximizing efficiency, and fostering rapid innovation. Speed to release has shifted from weeks to mere hours, thanks to our collaborative approach and operational efficiency,” said Raghavendra Pawar.
Traditional 3rd party payment integrity solution vendors exploit payment inaccuracies, which negatively impacts the provider’s experience and trust in payers and ends up ballooning waste and improper payments. With CoverSelf, payor payment integrity teams can reduce healthcare costs transparently and collaboratively with providers.
“Having worked with several of the largest health plans in the US, I have seen first-hand the unmet needs and improvement potential in their claims and payment integrity processes. That is why I am very excited to work with CoverSelf, which is the most innovative PI solution that I have come across. I firmly believe that not only is the next-gen, cloud-native, built-from-scratch platform that CoverSelf has created unique in its capabilities, CoverSelf’s value proposition of empowering payer internal PI teams to take back control from 3rd party vendors is also very appealing – several ex-clients who have met with CoverSelf have told me that this is the most differentiated offering that they have seen to date”, said Ashish Singh, ex-Global Healthcare Practice Leader and 30 year partner with Bain & Company.
CoverSelf’s purpose-built platform utilizes multiple approaches to reduce waste while identifying new savings opportunities. The platform empowers payers to adapt to claims and payment inaccuracies by enabling them to configure their policies and logic in simple English like language or use simple policy-specific templates, overcoming the fear of losing IP and fostering innovation and new concept releases without technical dependencies.
“CoverSelf is in the process of building pathbreaking features with GenAI. We aim to change how payment integrity is approached and executed with these cutting-edge features. Our vision remains steadfast–we want to empower payer PI teams and make them first-class citizens of payment integrity rather than have 3rd party vendors controlling it. Currently, GenAI is in stealth mode, and we are working with the stakeholders to add an outstanding and simplified user experience. With that said, we welcome our new investors and thank our existing backers for their continued confidence!” added Rajasekhar Maddireddy, Co-founder of CoverSelf
On added further capital Dirk Van Quaquebeke, Managing Partner, BEENEXT commented: “According to the Centers for Medicare and Medicaid (CMS), Americans spent $4.1 trillion on healthcare in 2020, of which an estimated $1.2 trillion can be attributed to some form of waste or abuse that leads to overcharges. CoverSelf’s vision to democratize the healthcare claims and payment integrity industry with their fully open and transparent solution built with a spirit of collaboration is truly inspirational,”
“By bringing the payment integrity solution in-house, CoverSelf shifts the control of payment integrity from traditional outside vendors to payers. As payers start using CoverSelf, they will progressively need fewer external payment integrity vendors. Ultimately, CoverSelf will be the only payment integrity platform anyone will ever need.” said Sonal Saldanha, VP, Investments, 3One4 Capital.